A ONCE-RARE genital super-fungus that can only be killed off with a ‘toxic’ treatment is now spreading among families across the UK, experts warn.
Cases of , previously almost unheard of in Britain, have surged by nearly 500 per cent in the past three years, leaving hundreds at risk of becoming “social pariahs”.
 Trichophyton indotineae can spread all over the bodyCredit: MDPI
Trichophyton indotineae can spread all over the bodyCredit: MDPI
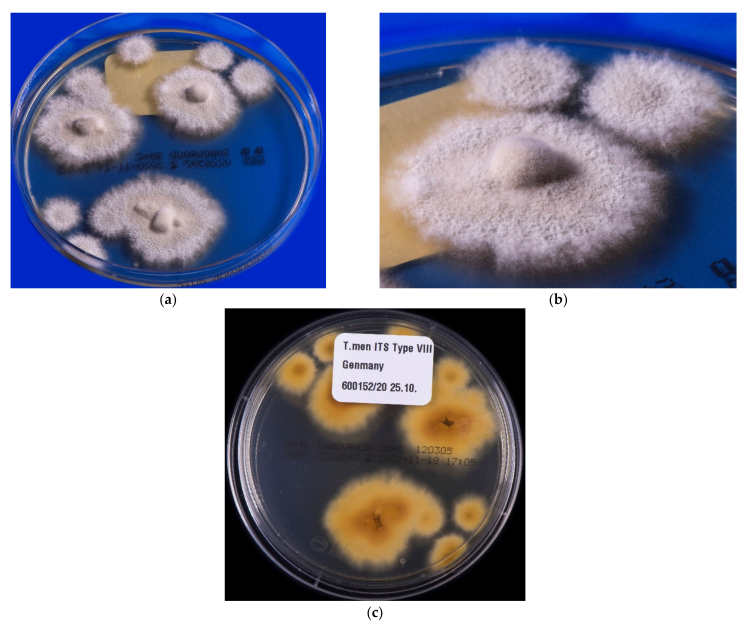 The fungus has become resistant to standard treatmentsCredit: MDPI
The fungus has become resistant to standard treatmentsCredit: MDPI
The infection isn’t life-threatening, but is notoriously hard to treat and can look severe and unsightly, spreading across the body so people feel to ashamed to leave their homes.
New data presented at the ESCAIDE conference in Poland last week [November 20] revealed that infections in the UK and Ireland have risen sharply in the past two years, climbing from just 44 before 2022 to 258 as of March this year [2025].
“It’s becoming a really big problem in the UK,” Professor Darius Armstrong-James, a fungal expert at Imperial College London, told The Sun.
“We don’t know how endemic, or pandemic, it will get here, but already, the growing frequency of new cases coming into hospitals is very concerning.”
The fungus, also known as T. indotineae, is a type of ringworm first reported in India in 2014, which has since mutated to withstand standard anti-fungal .
Nowadays, patients often end up needing months of hospital-based treatment with itraconazole, a drug that carries a risk of serious toxic side effects, particularly to the liver and heart.
It comes as many fungal pathogens, including candida, which causes common infections like vaginal , are becoming increasingly resistant to treatment.
T. indotineae causes “angry” and “formidable” red itchy rashes, Dr David Denning, an infectious diseases expert at the University of Manchester, said, mostly in the groin, thighs and buttocks according to the new research.
If left untreated, it spreads to other parts of the body – including the face – becoming painful, inflamed, vulnerable to infection and can cause permanent scarring.
“And it is very socially limiting,” Dr Denning added.
“Some people won’t feel like they can leave the house or go to work. They can become social pariahs.”
It can also be difficult to diagnose, Prof Armstrong-James said.
“It could be easily mistaken for eczema or psoriasis if tests are not conducted,” he said.
Over the last decade, the infection has spread to over 20 countries, including Germany and the US.
In the UK, most of the cases being reported are in people of South Asian heritage, according to the new data, collected by the UK Health Security Agency (UKHSA).
But Dr Denning said it “won’t be long” until it seeps into the wider population.
 Most case in the UK have been spotted on the groin, buttocks and thighsCredit: MDPI
Most case in the UK have been spotted on the groin, buttocks and thighsCredit: MDPI
 It can easily be mistaken for eczema or psoriasisCredit: Science Direct
It can easily be mistaken for eczema or psoriasisCredit: Science Direct What is antimicrobial resistance?
Antimicrobial resistance (AMR) is a global health and development threat.
Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
Source: WHO
“This is clearly going to become a big issue across the world,” he added.
Most patients were female and aged between 20 and 59, with the youngest case being just two years old.
T. indotineae spreads very easily through contaminated household items, like towels, bedding and clothing, and previous reports have linked it to sexual contact.
It can also spread in warm shared spaces such as gyms, changing rooms and steam rooms, where skin flakes linger.
“It’s something that we have noticed spreads in families,” Professor Armstrong-James explained.
“We’re seeing clusters. Once one person gets it, others follow,” he said.
The wait time to see an NHS dermatologist, in some regions, is just over 18 weeks.
“It means many people stay infectious for far longer than they should,” Dr Denning added.
“Major implications” for human health
Ever since the outbreak in 2020, experts have noticed an increase in deadly fungal diseases among hospitalised patients.
Earlier this year, over Candidozyma auris – a tough, drug-resistant fungus that has also been reported and can be deadly and spreads easily in hospitals.
Between 2013 and 2024, there were 637 reported cases of in England, with 178 just last year alone, data suggests.
Despite this, fungal infections receive very little attention and research resources.
As it stands, there are only four classes of antifungal medicines available and very few in development.
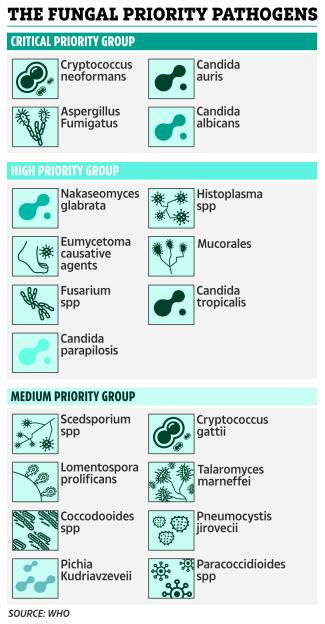
In 2022, the World Health Organization (WHO) published its list of 19 fungal priority pathogens to watch , warning that rising antifungal resistance has “major implications” for human health.
Ringworm: Everything you need to know
Ringworm is a common fungal infection that can cause a red or silvery ring-like rash on the skin.
It commonly affects arms and legs, but it can appear almost anywhere on the body.
Despite its name, ringworm doesn’t have anything to do with worms.
What does ringworm look like?
Signs typically appear between four and 14 days after your skin comes in contact with the fungi that cause ringworm, including:
- Circular, ring-shaped scales or plaques
- Flat patches with a raised, round border
- Itchy skin
- Hair loss or bald spots in the affected area
What causes ringworm?
Despite its name, a fungus causes ringworm.
This type of fungus naturally lives on your skin, hair and nails. However, when their environment gets hot and damp, the fungi start growing uncontrollably.
You can get this infection anytime your skin comes into contact with the ringworm fungus on someone else’s skin.
How contagious is ringworm?
Ringworm is contagious. It can live on your skin, on surfaces and in soil. The main ways ringworm spreads are:
- Skin-to-skin contact with a person who has ringworm
- Contact with an infected dog, cat or animal (livestock or pets)
- Contact with a contaminated surface, such as a locker room floor or sweaty gym clothes
- Sharing objects with an infected person or animal such as a brush, towel or bedding
- Contaminated soil
How is ringworm treated?
Several nonprescription (over-the-counter) and prescription antifungal medications are available to treat ringworm.
Antifungals come in various forms like creams, gels or powders.
Your healthcare provider can treat more widespread ringworm with oral antifungal medication.
However, trichophyton indotineae is a type of ringworm that is resistent to standard treatments.
Instead, patients end up needing months of hospital-based treatment with itraconazole, a drug that carries a risk of serious toxic side effects, particularly to the liver and heart.







